Ask MoneyTalk: How might healthcare practices evolve through COVID-19?
The COVID-19 pandemic has forced many healthcare professionals to rethink the ways they run their practices. Dr. Adam Stewart explains how he is triaging and scheduling patients now.

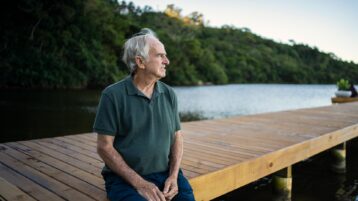
DR. ADAM STEWART
FAMILY PHYSICIAN
I know, I know. At times, I can feel the same way. “Another COVID-19 article?? Ugh.” Our newsfeeds these days are saturated with articles about the COVID-19 pandemic, many with very important information about your health and safety. Others verge on preaching to you about how you can live and improve your life during this pandemic.
I’m going to shift gears a little here. I’m not going to tell you how you can better use this time to find work-life balance. I’m not going to tell you this is a great time to pick up a new hobby.
Rather, I am going to mention some ways this pandemic has transformed workflows for how I am triaging and scheduling patients.
Many people are talking about how the COVID-19 pandemic has revolutionized the implementation of virtual care. This is true. But video-conferencing can’t be the entire solution. By necessity, we’ve had to revisit entirely the way we schedule patients. Perhaps surprisingly, I can see ways it could help me see more patients, and with appropriate timeliness. Ultimately, I think this could increase the capacity of my practice and the healthcare system in general, though it may also depend on some other shifts, which I’ll also explain.
New systems for same-day bookings
Like many clinics, we have offered same-day booking for years. There are many variants of this concept, but the gist of it is that doctors leave most of their daily appointment spots empty for patients who call in that day and need to be seen.
One of the drawbacks to this, though, is that access can be too good. What!? You ask? How could that be? Well, not every concern needs to be seen that very same day. And perhaps some concerns need not be seen in person at all.
The problem, I was finding, is that my days were often becoming filled with visits that didn’t need to be seen right away or didn’t require being seen in person. Later that morning, other patients would call in with issues that did need to be seen, but all those same-day spots had been booked.
Well before the COVID-19 pandemic, I started to think: If only I could be the one answering the phone first thing in the morning when that flood of calls comes in. As the family doctor, I know my patients best. I am in the best position to gauge whether that particular patient needs to be seen today versus a patient who could perhaps wait.
Further, I often thought: If I could have offered that patient a quick couple of minutes of advice over the phone, then that could have saved an entire 20-minute visit for someone else that day. I would imagine myself answering the flood of phone calls for the first half hour in the morning, like the conductor of an orchestra, directing where and when everything should fit into its place — both by urgency and modality of visit.
When the COVID-19 pandemic was thrust upon us, we immediately stopped automatically booking patients for in-person visits. Quite abruptly, we had a version of the following model in action.
Staff answered patients’ calls and took preliminary details (including screening for COVID-19 symptoms and risks), then messaged me for direction. I decided how best to handle each particular concern or request. There were several options I could take:
- Call the patient directly
- Ask the staff to book a video visit
- Renew their prescription without seeing them
- Ask the patient to email or message me additional details and/or photos
- Decide the patient needs seen in person and have the staff book an appointment
In this workflow, I got to assess the urgency of the matter: If I was swamped that day, some of the concerns could be deferred until another day when things were less busy.
Improvements to build upon moving forward
This process has been far from perfect. It’s still new and requires some fine-tuning.
As I’ve written before, we need to leverage the power of delegation. It’s obvious to me that the doctor shouldn’t be physically answering phones on the front line. Staff can and should be the ones taking preliminary information.
From there, I can see there are opportunities for workflow processes to be developed and streamlined, especially for particular symptoms or concerns. We may also be cautious in implementing these developments, recognizing that nothing in medicine fits into nice tidy clear-cut algorithms.
New thinking for government and billings
There is the potential here to revolutionize patient bookings in a way that could increase the capacity of our practices and the overall healthcare system enormously.
One of the barriers, though, may be that most physicians are only paid to see patients in person. For the vast majority of us, phone calls, emails, and even video visits have not been compensated for. This was on the verge of improving before COVID-19, so hopefully this pandemic has fast-forwarded this issue as well.
As you can see, for this to succeed, physicians may need to be paid for more than just their the services they provide in person. If the COVID-19 pandemic is showing us how to increase capacity within our practices, this would have tremendous implications for both patient care and clinic revenues.
Adam Stewart is a family physician with a practice based in Madoc, Ontario. In 2017 he was named by the Canadian Medical Association as one of "17 physicians who have helped shape the future of health care." More information on his practice can be found at www.stewartmedicine.com.